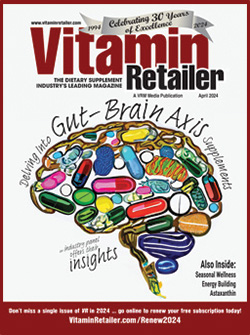
April Must Reads
Wellness for All Seasons
by Joy Choquette
Delving Into Gut-Brain Axis Supplements
by James Gormley
Customizing Energy Enhancement
by Lisa Schofield
Latest News
Thursday, Apr. 18, 2024
Natural Path Silver Wings Celebrates its 30-year Anniversary
by Eric Munson
Deep Dive Into Our Current Issue
with our monthly exclusives & columns
Columns:
VR Spotlight
Don't Miss Out!
Industry Professionals
Stay Informed!
Stay informed about the latest health, nutrition, and wellness developments by signing up for a FREE subscription to 'Vitamin Retailer' magazine.
Advertisers
Get your brand and products in front of over 9,340+ health, nutrition, and wellness professionals every month by advertising in Vitamin Retailer print magazine, and 7,790+ professionals in our weekly enewsletter.











![[Sponsored Video] Visit HP Ingredients at Natural Products Expo West 2024](https://vitaminretailer.com/wp-content/uploads/2024/04/sponsored-video-visit-hp-ingredi-768x432.jpg)
![[Extra! Extra!] New Help for Hay Fever Sufferers](https://vitaminretailer.com/wp-content/uploads/2024/03/SeasonalWellness-768x361.jpg)
![[Extra! Extra!] Talking Gut-Brain Axis Nutrition With NOW’s Neil Levin](https://vitaminretailer.com/wp-content/uploads/2024/03/GutBrainAxis-768x334.jpg)
![[Extra! Extra!] Ketone Supplements May Worsen Performance in Endurance Athletes](https://vitaminretailer.com/wp-content/uploads/2024/03/EnergyBuilding-768x512.jpg)
![[Extra! Extra!] Researchers Find Link Between NAD+ and Impaired Women’s Fertility](https://vitaminretailer.com/wp-content/uploads/2024/02/Womens-Health-768x495-1709222099.jpg)
![[Extra! Extra!] Talking Sports and Active Nutrition With Carl Germano](https://vitaminretailer.com/wp-content/uploads/2024/02/Sports-Nutrition-768x512-1709222045.jpg)




